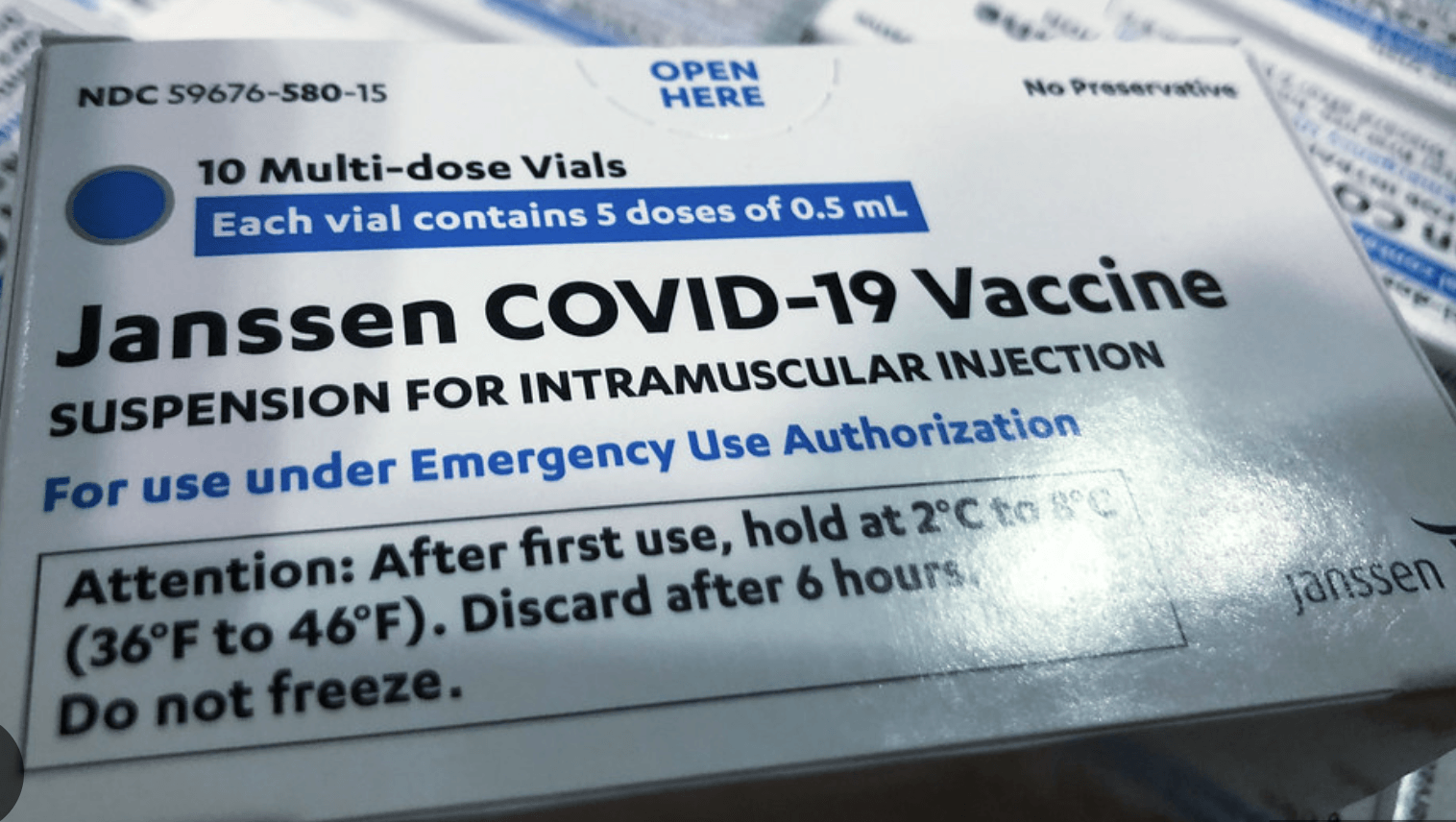
ARS TECHNICA – The Food and Drug Administration has withdrawn authorization for Johnson & Johnson’s COVID-19 vaccine, ending its short-lived but troubled existence amid the pandemic.
In a letter last week, the FDA’s top vaccine regulator, Peter Marks, wrote to Janssen Biotech—the Johnson & Johnson-owned, Belgium-based company responsible for the vaccine—saying that the agency was revoking authorization.
Marks opened the letter by noting that the withdrawal was at the request of the company.
According to Marks, Janssen’s May 22 letter informed the FDA that:
“the last lots of the Janssen COVID-19 Vaccine purchased by the United States Government have expired, that there is no demand for new lots of the Janssen COVID-19 Vaccine in the United States, and that Janssen Biotech, Inc does not intend to update the strain composition of this vaccine to address emerging variants.”
Last month, the Centers for Disease Control and Prevention noted on its website that the vaccine was no longer available in the US because the remaining government stock expired on May 7, 2023.
According to CDC data tracking, about 31.5 million J&J vaccine doses had been delivered to states amid the pandemic, but only around 19 million were administered, leaving the remaining 12.5 million or so to expire.
The beginning of the end for the once-promising single-dose vaccine came just weeks after its FDA authorization on February 27, 2021.
On March 13, 2021, the FDA and CDC paused the use of the J&J vaccine out of concern for an extremely rare clotting disorder, which was first noticed with a similar vaccine made by AstraZeneca. Both vaccines used an adenovirus vector-based design, though the AstraZeneca vaccine was never authorized for use in the US.
The pause on J&J’s vaccine lasted just 11 days, but the damage was done, and demand for the vaccine tumbled, never to recover.
Meanwhile, US production of the vaccine was mired by the scandal surrounding Emergent BioSolutions, a government contractor that ruined tens of millions of J&J COVID-19 vaccine doses due to quality-control problems and contamination.
Despite raking in hundreds of millions of dollars from government contracts, Emergent had a history of manufacturing violations …