Views from 4 sources:
-
OSF HealthCare: COVID-19 and the flu are not the same
-
Mayo Clinic: What’s the difference between COVID-19 and the flu?
-
The Lancet: Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics
-
WHO: Coronavirus disease (COVID-19): Similarities and differences with influenza
COVID-19 and the flu are not the same
OSF HealthCare is an integrated health system owned and operated by The Sisters of the Third Order of St. Francis, Peoria, Illinois. OSF HealthCare employs more than 23,600 people in 147 locations, including 14 hospitals, throughout Illinois and Michigan. The OSF HealthCare physician network employs more than 1,500 primary care, specialists, and advanced practice providers.
October 3, 2020
OSF HealthCare – Even with more than 1 million deaths worldwide and 210,000 in the United States, the notion persists that COVID-19 is just another flu.
Not true, said Clifford Martin, MD, vice president and chief medical officer of OSF HealthCare St. Mary Medical Center in Galesburg, Illinois. The novel coronavirus known as SARS-CoV-2, which causes COVID-19, is significantly different from influenza.
“It’s a highly contagious virus, and it’s a much deadlier virus,” Dr. Martin said.
Major differences between flu and COVID-19
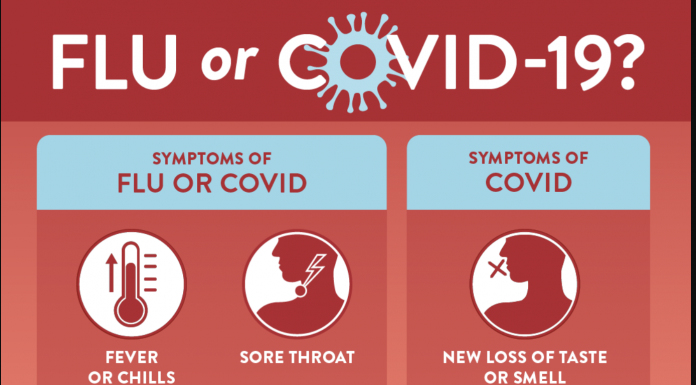
There are many similarities between COVID-19 and the flu. Both attack the respiratory system and present the same type of symptoms, such as fever, cough, sore throat, and congestion.
COVID-19 also can be marked by breathing difficulty, loss of taste and smell, nausea, vomiting and diarrhea. It attacks the respiratory and neurological systems (lungs and brain), as well as the heart, kidneys, and other organs.
The flu and COVID-19 differ in additional ways.
“When COVID-19 starts to come on, it’s a little more delayed,” Dr. Martin said. “There is often a phase where it’s just more of the mild systems, and then a week later, it starts to intensify.
“It really seems to create a much more intense inflammatory response in the body. The virus overwhelms the system, causing blood clotting and scarring. It does have some really long-lasting effects, particularly for those individuals who get the most ill.”

Influenza can overwhelm a person, too, and even land them in the intensive care unit (ICU).
“But each year when we see that with influenza, we see what we call normal ICU progression – two or three days in ICU and they start to improve,” Dr. Martin said. “Maybe they go to a less intensive care bed for a little while and then home. But folks with COVID-19, sometimes we see weeks on end of needing ICU care, and then ultimately, sometimes lives are lost.”
Influenza can also kill, but the mortality numbers are exponentially smaller than COVID-19 deaths. Dr. Martin said an estimated 28,000 Americans died from influenza during the 2018-19 flu season. That’s about 14% of the number who died during the first six months of the pandemic. Source.
What’s the difference between COVID-19 and the flu?
Oct. 10, 2020
Mayo Clinic – COVID-19 and the flu have several differences. COVID-19 and the flu are caused by different viruses. COVID-19 is caused by a new coronavirus called SARS-CoV-2, while influenza is caused by influenza A and B viruses.
Symptoms of COVID-19 and the flu appear at different times and have some differences. With COVID-19, you may experience loss of taste or smell. COVID-19 symptoms generally appear two to 14 days after exposure.
Flu symptoms usually appear about one to four days after exposure. COVID-19 appears to be more contagious and to spread more quickly than the flu. Severe illness such as lung injury may be more frequent with COVID-19 than with influenza. The mortality rate also appears to be higher with COVID-19 than the flu.
COVID-19 can cause different complications from the flu, such as blood clots and multisystem inflammatory syndrome in children.
Another difference is that the flu can be treated with antiviral drugs. No antiviral drugs are currently approved to treat COVID-19. Researchers are evaluating many drugs and treatments for COVID-19. Some drugs may help reduce the severity of COVID-19.
You can get an annual flu vaccine to help reduce your risk of the flu. The flu vaccine can also reduce the severity of the flu and the risk of serious complications. Each year’s flu vaccine provides protection from the three or four influenza viruses that are expected to be the most common during that year’s flu season. The vaccine can be given as a shot (injection) or as a nasal spray.
The flu vaccine doesn’t protect you from getting COVID-19. Research also shows that getting the flu vaccine does not make you more likely to get COVID-19 or other respiratory infections.
No vaccine is currently available for the virus that causes COVID-19. But researchers are working to develop vaccines to prevent COVID-19. Source.
Comparing SARS-CoV-2 with SARS-CoV and influenza pandemics
Published: July 03, 2020 (Document is current as of 11/3/21020)
The Lancet – The SARS-CoV-2 pandemic has already caused severe morbidity and mortality in older adults, much higher than in the pandemic influenza. Although children are clearly less affected, their role in the transmission of the virus still needs to be studied.
At this early stage in the pandemic, there are no effective treatments such as antivirals or passive immunization schemes. Development of a safe and effective vaccine will take time. Thus, only supportive treatment in hospitals is currently available, and efforts to slow and limit the spread of the virus continue. The goal is to reduce the impact of the virus, prevent overwhelming the health-care system, and protect the people at highest risk of severe outcomes while waiting for an effective vaccine and treatments.
Historical evidence from influenza pandemics which occurred in the past century shows us that pandemics tend to come in waves over the first 2–5 years as the population immunity builds-up (naturally or through vaccination), and then the number of infected cases tends to decrease. This observation is the most likely trajectory for the SARS-CoV-2 virus.
However, the near future will require a transition to a new normal, in which a combination of physical distancing, enhanced testing, quarantine, and contact tracing will be needed for a long time.
While clinical research and testing of antivirals and vaccine candidates is ongoing, scientists will learn from regions and countries that were first affected. Also, epidemiological and phylogenetic studies can yield much information about risk factors (other than age) such as disease transmission, the role of children in transmission, and a better estimate of case fatality.
It is highly likely that after SARS-CoV-2 there will be another pandemic.
It might be another coronavirus, an influenza virus, a paramyxovirus, or a completely new disease. We believe that learning from this experience is crucial so that we can meet a future pandemic threat with far better preparation in terms of testing, adequate stocks of personal protective equipment, and critical care capability.
International pandemic planning is needed to ensure collaboration between countries, including better surveillance of emerging infections especially zoonoses. Controlling an outbreak has everything to do with mitigating casualties such as economic losses, joblessness, loneliness, and even loss of human dignity at the end of life. Source.
Coronavirus disease (COVID-19): Similarities and differences with influenza
17 March 2020
World Health Organization – As the COVID-19 outbreak continues to evolve, comparisons have been drawn to influenza. Both cause respiratory disease, yet there are important differences between the two viruses and how they spread. This has important implications for the public health measures that can be implemented to respond to each virus.
How are COVID-19 and influenza viruses similar?
Firstly, COVID-19 and influenza viruses have a similar disease presentation. That is, they both cause respiratory disease, which presents as a wide range of illness from asymptomatic or mild through to severe disease and death.
Secondly, both viruses are transmitted by contact, droplets, and fomites. As a result, the same public health measures, such as hand hygiene and good respiratory etiquette (coughing into your elbow or into a tissue and immediately disposing of the tissue), are important actions all can take to prevent infection.
How are COVID-19 and influenza viruses different?
The speed of transmission is an important point of difference between the two viruses. Influenza has a shorter median incubation period (the time from infection to appearance of symptoms) and a shorter serial interval (the time between successive cases) than COVID-19 virus. The serial interval for COVID-19 virus is estimated to be 5-6 days, while for influenza virus, the serial interval is 3 days. This means that influenza can spread faster than COVID-19.
Further, transmission in the first 3-5 days of illness, or potentially pre-symptomatic transmission –transmission of the virus before the appearance of symptoms – is a major driver of transmission for influenza. In contrast, while we are learning that there are people who can shed COVID-19 virus 24-48 hours prior to symptom onset, at present, this does not appear to be a major driver of transmission.
The reproductive number – the number of secondary infections generated from one infected individual – is understood to be between 2 and 2.5 for COVID-19 virus, higher than for influenza. However, estimates for both COVID-19 and influenza viruses are very context and time-specific, making direct comparisons more difficult.
Children are important drivers of influenza virus transmission in the community. For COVID-19 virus, initial data indicates that children are less affected than adults and that clinical attack rates in the 0-19 age group are low. Further preliminary data from household transmission studies in China suggest that children are infected from adults, rather than vice versa.
While the range of symptoms for the two viruses is similar, the fraction with severe disease appears to be different. For COVID-19, data to date suggest that 80% of infections are mild or asymptomatic, 15% are severe infection, requiring oxygen and 5% are critical infections, requiring ventilation. These fractions of severe and critical infection would be higher than what is observed for influenza infection.
Those most at risk for severe influenza infection are children, pregnant women, elderly, those with underlying chronic medical conditions, and those who are immunosuppressed. For COVID-19, our current understanding is that older age and underlying conditions increase the risk for severe infection.
Mortality for COVID-19 appears higher than for influenza, especially seasonal influenza. While the true mortality of COVID-19 will take some time to fully understand, the data we have so far indicate that the crude mortality ratio (the number of reported deaths divided by the reported cases) is between 3-4%, the infection mortality rate (the number of reported deaths divided by the number of infections) will be lower.
For seasonal influenza, mortality is usually well below 0.1%. However, mortality is to a large extent determined by access to and quality of health care.
What medical interventions are available for COVID-19 and influenza viruses?
While there are a number of therapeutics currently in clinical trials in China and more than 20 vaccines in development for COVID-19, there are currently no licensed vaccines or therapeutics for COVID-19. In contrast, antivirals and vaccines available for influenza. While the influenza vaccine is not effective against COVID-19 virus, it is highly recommended to get vaccinated each year to prevent influenza infection.
ALSO ON HEADLINE HEALTH TODAY: Biden’s Failing Health Assures Huge Trump Win | Swing-State Doctors Target Trump | Ghislaine Evidence Deadline Looms